Interoperability – Building a Roadmap
Healthcare Triangle
Mar 16, 2021
Where will the road take us? Are we there yet? Familiar phrases amongst road-trippers and travelers, but it’s not a strategy for Healthcare Interoperability. This road needs to be planned out and built with flexibility; a framework for what the future may bring. Consider the interstate road systems across North America. It cannot get you everywhere you want to go, but it provides a route to get you most of the way there that is efficient and provides services along the way.
Before we hit the road, let’s remember where we have been.
Our interoperability journey began over 30 years ago. Initially taking the form of exporting patient administrative data to flat files, proprietary streams of data, and perhaps unique ODBC drivers to access one-off databases. As healthcare systems evolved beyond the patient register to include billing and documentation, these methods became increasingly demanding for IT professionals.
In 1987, Health Level 7 (HL7) began the build toward a unified messaging standard and solution set. This platform has been widely adopted in various versions (predominantly version 2.3-2.6) by vendors and health systems over the past 30 years. The HL7 2.x standard is a mature model around patient activity and use case scenarios. It provides a specific framework for exact data elements to be sent and expected between two systems.
Over the past decade in the US, the ONC produced a shared roadmap vision to achieve “interoperability". This did supply healthcare with a roadmap, which was successful as its own project. Certified EHRs were implemented allowing for patient portal access, meaningful use measures were implemented and enforced to a degree, and the ISA continues to provide guidance on standards usage. Also during this era, HL7 produced the FHIR standards as the next generation of integration tools as APIs enter the healthcare IT spectrum.
“No matter where you go, there you are” - Buckaroo Banzai
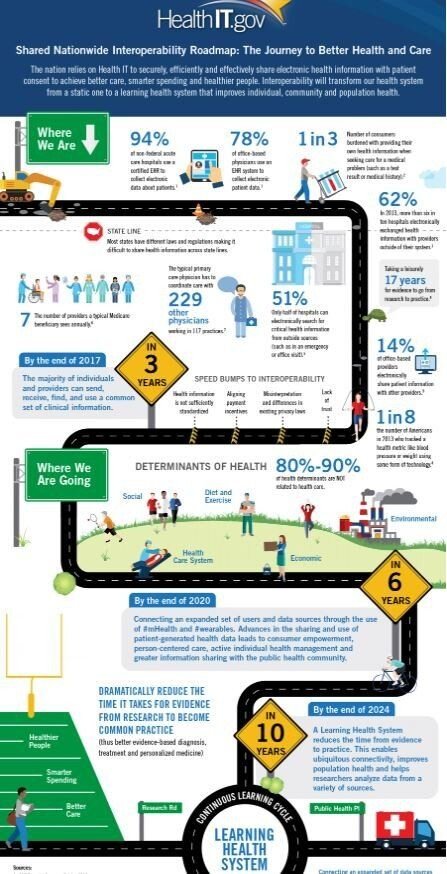
The perceived success of the ONC roadmap outcomes has been questionable to some. There is no doubt, the amount and type of healthcare data available now for exchange has greatly increased in the past decade because of these roadmap initiatives. However, a lot of effort and money was spent on some platforms with questionable payoffs.
- How widely is direct messaging used by physicians? Many hospitals claim it is only used to qualify for the MU measure!
- Data is constantly being pumped into HIEs. How much is retrieved and incorporated into the EHR record and then accessed by your physician?
- How many extra steps is it taking to analyze “outside” data, format it correctly, tag it and consume it?
- How many duplicate CCDs and discrete data results are there in the HIE that are now in your EHR? Med lists, procedures, diagnoses, labs, etc...
The 21st Century Cures Act promotes the patient being in the center - supplied with secured access and basic tools to get to their data using APIs. This is a good thing for the patient when :
- Their data is accurate and available,
- Hospital pricing transparency is truly “transparent”,
- And their providers are ready to answer different, specific questions.
Patients can now read notes entered by their providers. Will they understand the terminology and abbreviations? How will this change the patient/doctor relationship?
Patients may also ask if they can get a comparable MRI down the street instead because their price is 60% cheaper. Is it the same test? How will their provider get the results if it’s outside their network?
Developers of integration and APIs will be working furiously to meet the consumer demands and data requests. Is there a way to leverage all of this for the hospital and create an edge over the competition?
Be roadworthy and not road weary
Is your hospital organization ready to “give up” its stance that “we created the data therefore we own it”? As patients acquire “their” healthcare data, what can your organization envision as the reasons your patients will stay engaged with you and come back to you for service?

At Healthcare Triangle, we’re adept drivers of strategic healthcare technological progress. We worked with Google to develop its , and partnered Interoperability Readiness Program with over 100 hospitals and 5 major pharmaceutical companies to implement breakthrough HIT solutions.
We can guide you on your path to interoperability. As technically proficient, digital transformation advisors for leading healthcare organizations, we’re experienced in accelerating progress. We understand how to merge necessary Healthcare IT goals with your strategic business objectives. HCTI can support you through this change and get it done securely, compliantly, and quickly.
In my next article, we will outline cloud strategies for your healthcare organization that can incorporate your existing integration investments and leverage the power of rapid API deployments and leveraging FHIR resources.
For further discussion or immediate healthcare project-related assistance, drop an email to info@healthcaretriangle.com or schedule a consultation.
Sources:



